A key provision of the Transparency in Coverage Rule requires health insurers and group health plans to post publicly available machine-readable files (MRFs) of all provider payment information. The MRFs must include in-network (INN) negotiated payment rates based on every provider agreement in force, including INN and extended networks for each group, plan and network offering; and historical out-of-network (OON) reimbursement rates for covered items and services. The MRF data must be updated monthly and made publicly available.
We’re implementing access to TTM Technologies, Inc. MRFs in accordance with the July 1, 2022, deadline. Beginning July 1, users will be able to access the MRF landing page below by clicking on the Transparency in Coverage link on the Anthem website at TTM Technologies, Inc..
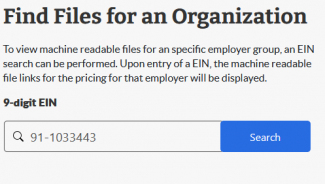
To access all files go to https://www.anthem.com/ca/machine-readable-file/search/ and enter the TTM EIN for access to all files.